"If I sit
silently, I have sinned."
- Mohammed Mossadegh
Many health care providers in Ebola-affected areas were infected and died because of inadequate supplies of PPE. Some health workers fled out of fear of becoming infected. Because health care workers are now focusing their efforts on the Ebola response, routine health care services have been interrupted. Obstetric and midwifery services are unavailable to many women because of the high risk of Ebola transmission during childbirth.
Baize, S., Pannetier, D., Oestereich, L., Rieger, T., Koivogui, L., Magassouba, N., et al. (2014). Emergence of Zaire Ebola virus disease in Guinea. New England Journal of Medicine, 371(15),1418-1425. doi:10.1056/NEJMoa1404505.
Centers for Disease Control and Prevention. (September 26, 2014). Estimating the future number of cases in the Ebola epidemic – Liberia and Sierra Leone, 2014-2015. Morbidity and Mortality Weekly Report, 63(03), 1-14. http://www.cdc.gov/mmwr/preview/mmwrhtml/su6303a1.htm.
- Mohammed Mossadegh
I arrived home a week ago yesterday. This is day 8 of my
21-day direct active monitoring. My last contact with a patient with Ebola virus disease
(EVD) was 13 days ago. Schieffelin and colleagues (2014) estimated
that the incubation period (time from exposure to the virus to onset of
symptoms) for EVD in Sierra Leone was 6 to 12 days. The WHO Ebola Response Team
(2014)
estimated the mean (average) incubation period to be 11.4 days. My risk of becoming
infected with ebolavirus while wearing personal protective equipment (PPE) was
low and my certainty that I am not infected increases with each passing day.
Unlike some of my colleagues who live in other states, I am
not "quarantined" and no restrictions on my movements have been
imposed by either the Washington State Department of Health or my local health
department - my employer. Yesterday was my first day back at the health
department since I left for the CDC Ebola safety training seven weeks ago. I was surprised the first time
someone extended a hand for me to shake, a gesture that is discouraged
during an epidemic of EVD.
Holly suggested that I post more stories about the patients
I saw in Sierra Leone. The problem is that I really don't know the stories of
most of our patients. We received very little information about our patients at
the time they were admitted and most of my time in the confirmed ward was spent
attending to people who were usually too sick to talk. I had only enough time
to make small talk with the survivors who were waiting to be discharged. The
only story I have to tell is my own.
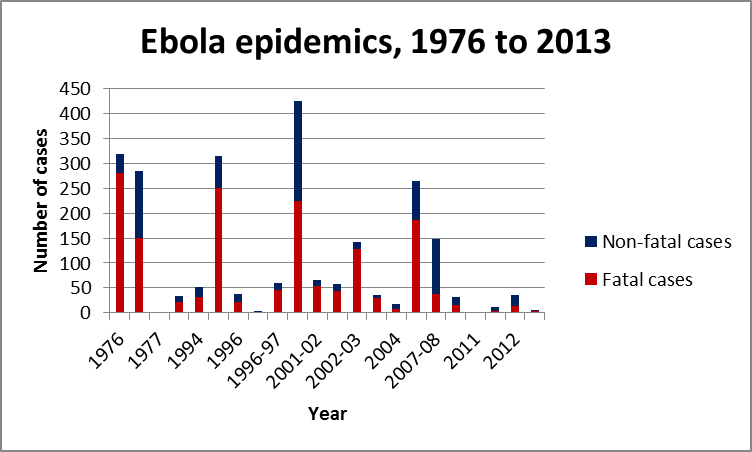
Then there are the stories that the numbers tell us.
Baize et al. (2014) traced the
Ebola epidemic in West Africa to a 2-year-old child in Guinea who died from the disease
December 6, 2013. With the exception of a single human case of Taï Forest ebolavirus from a chimpanzee in Ivory Coast in 1994, there had never
been an outbreak of EVD in West Africa.
On March 10th of this year, the World Health
Organization (WHO) was notified of an outbreak of an unknown infectious disease
characterized by fever, vomiting, and diarrhea in Guinea. A few days later, Zaire ebolavirus was identified in blood
from patients who were hospitalized with the disease. The disease spread to Liberia in March and to Sierra Leone in May. On August 8th, the WHO declared the Ebola epidemic in West Africa a Public Health Emergency of International Concern. At that time, 1,779 cases and 961 deaths due to EVD had been
reported to WHO. By the end of the month, the number of cases and deaths
exceeded the total numbers of cases and deaths from all previous EVD epidemics
combined.
 |
| CDC |
The interventions used to contain an outbreak of EVD are the
same as those used for other communicable diseases. The challenge has been
implementing those strategies in places with very limited health care
resources.
|
Country
|
Nurses and midwives per 1,000 population
|
Physicians per 1,000 population
|
|
Guinea
|
0.511
|
0.1
|
|
Liberia
|
0.274
|
0.014
|
|
Sierra Leone
|
0.166
|
0.022
|
|
United States of America
|
9.815
|
2.452
|
|
| ||
Many health care providers in Ebola-affected areas were infected and died because of inadequate supplies of PPE. Some health workers fled out of fear of becoming infected. Because health care workers are now focusing their efforts on the Ebola response, routine health care services have been interrupted. Obstetric and midwifery services are unavailable to many women because of the high risk of Ebola transmission during childbirth.
This epidemic is not over. The Sierra Leone Ministry of
Health and Sanitation estimated that the crude reproduction number for EVD in
that country remains above 1, which means that every person with EVD can be
expected to infect at least one other person. Transmission of the disease will
be sustained until the reproduction number drops below one.
 |
 |
| Number of new Ebola virus disease cases reported, by epidemiologic week — three countries, West Africa, March 29–November 30, 2014 (CDC) |
 |
| Number of new cases of Ebola virus disease reported — Guinea, Liberia, and Sierra Leone, November 9–30, 2014 (CDC) |
I started this blog nearly three years ago. On October 14th of this year, a week after my first post on Ebola virus disease (EVD), this blog had 10,000 page views.
Now there are over 13,000 page views. Roughly a quarter of all of the hits on
this blog have happened in the last 11 weeks.
It seems that what I began as my
effort to keep my friends and family informed about my work in Sierra Leone got
the attention of far more people than I had anticipated. I was encouraged to
know that there were so many people reading this blog and am very grateful for
the support that I have received from people who have read my posts.
As the title suggests, this blog was intended to be a forum
for discussions about vaccines and vaccine-preventable diseases. I don't mean to minimize the importance of
the current Ebola epidemic, but I will end this post by bringing the discussion
back to vaccine-preventable diseases.
This epidemic dwarfs all previous EVD epidemics. This should
serve as a warning that every EVD epidemic deserves an immediate and decisive
response. As I write this, there have been a total of 19,463 cases and EVD and
7,573 deaths in Guinea, Liberia, and Sierra Leone.
In 2009, there were an estimated 79,292 cases of meningococcal disease in the African Meningitis Belt. The World
Health Organization estimates that there were 145,700 deaths from measles in
2013. There were 610 cases of measles in the U.S. between January 1 and November 29, 2014, the highest number of cases since measles was eliminated from the U.S. Most
of cases of measles in the U.S. are in people who have not been vaccinated
against the disease and most are associated with importation of the virus from
countries with low measles immunization coverage.
On the other hand, these numbers are small compared to the
millions of deaths due to liver disease prevented by routine hepatitis B
vaccination in China (Hadler et al., 2013).
The current EVD epidemic began as a small outbreak in a
remote part of Africa and became an international public health emergency. Yet,
there are tens of thousands more deaths from vaccine-preventable diseases every
year than there have been deaths from EVD since the disease was first
identified 38 years ago. Those deaths deserve our attention too.
Merry Christmas!
 |
| Andrew with his Grandpa Esvelt |
References
Baize, S., Pannetier, D., Oestereich, L., Rieger, T., Koivogui, L., Magassouba, N., et al. (2014). Emergence of Zaire Ebola virus disease in Guinea. New England Journal of Medicine, 371(15),1418-1425. doi:10.1056/NEJMoa1404505.
Bernstein, L. (September 20, 2014). With Ebola crippling the health system, Liberians die of routine
medical services. Washington Post. http://www.washingtonpost.com/world/africa/with-ebola-crippling-the-health-system-liberians-die-of-routine-medical-problems/2014/09/20/727dcfbe-400b-11e4-b03f-de718edeb92f_story.html.
Briand, S., Bertherat, E., Cox, P., Formenty, P., Kieny,
M-P., Myhre, J. K., et al. (2014). The international Ebola emergency. New England Journal of Medicine, 371(13),
1180-1183. doi:10.1056/NEJMp1409858.
Boozary, A. S., Farmer, P. E., & Jha, A. K. (2014). The
Ebola outbreak, fragile health systems, and quality as a cure. JAMA, 312(18), 1859-1960. doi:10.1001/jama.2014.14387.
Centers for Disease Control and Prevention. (June 6, 2014).
Measles – United States, January 1 – May 23, 2014. Morbidity and Mortality Weekly Report, 63(22), 496-499. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6322a4.htm.
Centers for Disease Control and Prevention. (October 10,
2014). Assessment of Ebola virus disease, health care infrastructure, and
preparedness – four counties, Southeastern Liberia, August 2014. Morbidity and Mortality Weekly Report,
63(40), 891-893. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6340a3.htm.
Centers for Disease Control and Prevention. (September 26, 2014). Estimating the future number of cases in the Ebola epidemic – Liberia and Sierra Leone, 2014-2015. Morbidity and Mortality Weekly Report, 63(03), 1-14. http://www.cdc.gov/mmwr/preview/mmwrhtml/su6303a1.htm.
Centers for Disease Control and Prevention. (December 12,
2014). Ebola virus disease in health care workers – Sierra Leone, 2014. Morbidity and Mortality Weekly Report,
63(49), 1168-1171. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6349a6.htm.
Centers for Disease Control and Prevention. (December 12,
2014). Rapid assessment of Ebola infection prevention and control needs – six
districts, Sierra Leone, October 2014. Morbidity
and Mortality Weekly Report, 63(49), 1172-1174. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6349a7.htm.
Centers for Disease Control and Prevention. (December 19,
2014). Update: Ebola virus disease epidemic – West Africa, December 2014. Morbidity and Mortality Weekly Report,
63(50), 1199-1201. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6350a4.htm.
Doucleff, M. (November 18, 2014). Dangerous deliveries: Ebola leaves moms and babies without care.
NPR. http://www.npr.org/blogs/goatsandsoda/2014/11/18/364179795/dangerous-deliveries-ebola-devastates-womens-health-in-liberia.
Gire, S. K., Goba, A., Anderson, K. G,. Sealfon, R. S. G.,
Park, D. J., Kanneh, L., et al. (2014). Genomic surveillance elucidates Ebola
virus origin and transmission during the 2014 outbreak. Science, 345(6202), 1369-1372. doi:10.1126/science.1259657.
Hadler, S. C., Fuqiang, C., Averhoff, F., Taylor, T.,
Fuzhen, W., Li, L., et al. (2013). The impact of hepatitis B vaccine in China
and in the China GAVI Project. Vaccine,
31(Supple. 9), J66-J72. doi:10.1016/j.vaccine.2013.03.043.
Ministry of Health and Sanitation, Republic of Sierra Leone.
(6 December 2014). Weekly Ebola surveillance report. http://health.gov.sl/?p=1692.
Schieffelin, J. S., Shaffer, J. G., Goba, A., Gbakie, M.,
Gire, S. K., Colubri, A., et al. (2014). Clinical illness and outcomes in
patients with Ebola in Sierra Leone. New
England Journal of Medicine, 371(22), 2092-2100. doi:10.1056/NEJMoa1411680
World Health Organization. (2014). Number of suspected
meningitis cases and deaths reported: highlight on 2009 epidemiological season.
http://www.who.int/gho/epidemic_diseases/meningitis/suspected_cases_deaths_2009_text/en.
World Health Organization. (2014). WHO warns that progress
towards eliminating measles has stalled. http://www.who.int/mediacentre/news/releases/2014/eliminating-measles/en.
World Health Organization Ebola Response Team. (2014). Ebola
virus disease in West Africa – the first 9 months of the epidemic and forward
projections. New England Journal of
Medicine, 371(16), 1481-1495. doi:10.1056/NEJMoa1411100.